Post by Sam Donaldson (M.PhtySt, BAppSci(HMS), Physiotherapist APAM SMAM)
Recently, a patient presented with a lengthy (>3 month) history of lower back pain. This individual’s pain wouldn’t behave as typical lower back pain. There was also a complaint of some discomfort in other body regions that didn’t fit a typical spinal pain presentation. Upon being made aware of some recent illness, it became apparent that we might be dealing with something systemic or auto-immune.
Fortunately, these suspicions were justified once this patient attended a Rheumatologist, with a Spondyloarthropathy diagnosis being made and subsequent treatment being positive.
What was interesting in this case is the rarity of these patients and the challenge for the health professional that this type of patient presents from a diagnostic perspective.
It is, among other things, one of the Physiotherapists primary roles… ensuring that Physiotherapy treatment is appropriate for the patient in front of them. Through thorough questioning and examination of the patient in their initial appointment, we are essentially deciding whether we can help, and if not, what health professional might.
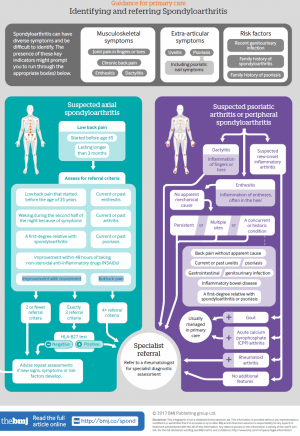
Fortunately, there are strong guidelines for the appropriate referral of a patient that we might suspect is suffering a Spondyloarthropathy. A recent “NICE Guideline” presented a number of clinical features of a patient’s presentation and at what point should a referral to a Rheumatologist be made. Bearing in mind (for any Physiotherapists reading), this might mean a phone call to the patient’s GP to discuss the possibility and for the referral to be made via the appropriate pathways.
One of the first decision for us to make is: is this patient suffering “Inflammatory Low Back Pain?” This is generally described as:
- Lower back pain lasting >3 months
- Better with movement and worse with rest
- Pain at night, improves upon getting up in morning
- Alternating buttock pain
- Insidious onset
Following the recognition of inflammatory lower back pain, a range of clinical features might also be present (see infographic). If 3 or more criteria are present, it is reasonable to be suspicious of a Spondyloarthropathy. Particularly since the average time between symptom onset and diagnosis is 8.5 years. This is a significant amount of time losing quality of life and suffering pain.
So, if this is the case for yourself or a loved one, a discussion with a primary health care provider such as your GP or Physiotherapist is certainly appropriate. For the Physiotherapists, hopefully some greater awareness and interest is sparked and further reading performed. We have a great role in assisting in musculoskeletal management of various spondyloarthropathies and the impact on our patient’s life can be astounding!
References:
McAllister, K., Goodson, N., Warburton, L., & Rogers, G. (2017). Spondyloarthritis: diagnosis and management: summary of NICE guidance. BMJ, 356, j839.
Akgul, O., & Ozgocmen, S. (2011). Classification criteria for spondyloarthropathies. World J Orthop, 2(12), 107-15.